What Is A Calcaneal Spur

Overview
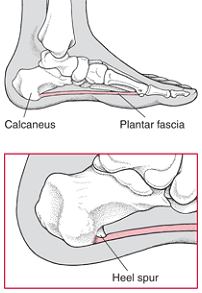
A heel spur is a bony projection on the sole (plantar) region of the heel bone (also known as the calcaneous). This condition may accompany or result from severe cases of inflammation to the structure called plantar fascia. This associated plantar fascia is a fibrous band of connective tissue on the sole of the foot, extending from the heel to the toes.
Causes
These bony protrusions are commonly found in association with a condition called Plantar Fasciitis. Plantar Fasciitis occurs when the plantar fascia ligament, which spans the arch of the foot, becomes stressed, torn and inflamed. Misalignment and excessive movement of the plantar fascia ligament is most typically the result of an abnormal walking gait. The ligament is designed to stretch with the bounce of each step you take, but if it stretches too much, the resulting small tears and inflammation can cause mild to extreme discomfort. At the same time, it is believed that heel spurs are formed as the body attempts to provide some additional support to the over-stretched ligament. In other words, calcium builds up as a prop to the plantar fascia.
Symptoms
The vast majority of people who have heel spurs feel the asscociated pain during their first steps in the morning. The pain is quite intense and felt either the bottom or front of the heel bone. Typically, the sharp pain diminishes after being up for a while but continues as a dull ache. The pain characteristically returns when first standing up after sitting for long periods.
Diagnosis
A thorough history and physical exam is always necessary for the proper diagnosis of heel spurs and other foot conditions. X rays of the heel area are helpful, as excess bone production will be visible.
Non Surgical Treatment
Acupuncture and acupressure can used to address the pain of heel spurs, in addition to using friction massage to help break up scar tissue and delay the onset of bony formations. Physical therapy may help relieve pain and improve movement. The Feldenkrais method could be especially helpful for retraining some of the compensation movements caused by the pain from the spur. Guided imagery or a light massage on the foot may help to relieve some of the pain. Other treatments include low-gear cycling, and pool running. Some chiropractors approve of moderate use of aspirin or ibuprofen, or other appropriate anti-inflammatory drugs. Chiropractic manipulation is not recommended, although chiropractors may offer custom-fitted shoe orthotics and other allopathic-type treatments.
Surgical Treatment
Almost 90% of the people suffering from heel spur get better with nonsurgical treatments. However, if the conservative treatments do not help you and you still have pain even after 9 to 12 months, your doctor may advise surgery for treating heel spur. The surgery helps in reducing the pain and improving your mobility. Some of the surgical techniques used by doctors are release of the plantar fascia. Removal of a spur. Before the surgery, the doctor will go for some pre-surgical tests and exams. After the operation, you will need to follow some specific recommendations which may include elevation of the foot, waiting time only after which you can put weight on the foot etc.
Prevention
In 2002, researchers attempted to compare the effects of various running techniques on pronation and resulting injuries like stress fractures and heel spurs. They suggested that it is possible to teach runners to stride in such a way as to minimize impact forces. One way is to lower running speed. Another is to take longer rest periods following a run.
Bursitis Of The Feet Pain Treatment
Bursitis and tendinitis are conditions that are also known as soft tissue rheumatic syndromes. A syndrome is a group of signs and symptoms that occur together and indicate a particular problem. This type of syndrome produces pain, swelling, or inflammation in the tissues and structures around a joint, such as the tendons, ligaments, bursae, and muscles.
Causes
Improper foot wear, tight shoes or shoes that do not fit properly can cause extra pressure and friction on the back of the heel. Overtime, this pressure causes irritation of the bursae that protects the Achilles tendon causing one or both to swell and become inflamed. Athletes who overtrain or runners that increase their distance to quickly are at greater risk of experiencing Achilles bursitis. With over use, the Achilles bursae and tendon can become irritated and inflamed leading to thickening of the bursae lining and wearing of the tendon. Fluid builds in the bursa when it becomes irritated causing swelling of the Achilles bursa and pain at the back of the heel.
Symptoms
Pain at the back of the heel at the attachment site of the Achilles tendon when running. Pain on palpation of the back of the heel or bottom of heel. Pain when standing on tiptoes. Swelling and redness at the back and bottom of the heel.
Diagnosis
Diagnosis is first by clinical suspicion of symptoms. This can be mistaken for gout or infection especially in the big toe region. A diagnosis of bursitis is usually used in combination of the underlying cause, for instance a bunion deformity, Haglund's deformity, or Heel Spur Syndrome. Many times the cause needs to be addressed to rid the problem of bursitis.
Non Surgical Treatment
For non-infectious bursitis, the preliminary treatment starts with non-operative options such as cold compression therapy and Blood Flow Stimulation Therapy. Surgery to remove the inflamed bursa is normally not required for bursitis, however if you fail to see improvement with the conservative treatments, your physician may recommend surgery to remove the bursa completely. Although this removes the problem of an inflamed bursa, you are left with less cushioning in your joint which can lead to a host of other conditions.
Surgical Treatment
Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.
How To Treat Hammer Toes Without Surgery
 Overview
Overview
hammertoe, Claw and Mallet Toe are similar conditions, all caused by deformity of the toe joints. They usually develop slowly from wearing poor fitting shoes, but can also be due to muscle or nerve damage. Muscle imbalance causes the toes to bend into odd positions which can be extremely painful, limiting walking and activity. They become more common with aging and affect approximately 10-15% of the population. Women are five times more likely to suffer from hammer, claw or mallet toe than men.
Causes
Factors that may increase you risk of hammertoe and mallet toe include age. The risk of hammertoe and mallet toe increases with age. Your sex. Women are much more likely to develop hammertoe or mallet toe than are men. Toe length. If your second toe is longer than your big toe, it's at higher risk of hammertoe or mallet toe.
 Symptoms
Symptoms
People who have painful hammertoes visit their podiatrist because their affected toe is either rubbing on the end their shoe (signaling a contracted flexor tendon), rubbing on the top of their shoe (signaling a contracted extensor tendon), or rubbing on another toe and causing a painful buildup of thick skin, known as a corn.
Diagnosis
Your doctor is very likely to be able to diagnose your hammertoe simply by examining your foot. Even before that, he or she will probably ask about your family and personal medical history and evaluate your gait as you walk and the types of shoes you wear. You'll be asked about your symptoms, when they started and when they occur. You may also Hammer toe be asked to flex your toe so that your doctor can get an idea of your range of motion. He or she may order x-rays in order to better define your deformity.
Non Surgical Treatment
Try to find shoes that are soft, roomy, and comfortable and avoid tight shoes or shoes with high heels. A shoe repair shop may be able to stretch a small pocket in regular shoes to make room for the hammertoe. Have a professional pedicure. Sometimes a skilled manicurist can file down a painful corn. Follow your healthcare provider's instructions. Ask your provider what activities you should avoid and when you can return to your normal activities, how to take care of yourself at home, what symptoms or problems you should watch for and what to do if you have them. Make sure you know when you should come back for a checkup.
Surgical Treatment
If these treatments are not sufficient at correcting the hammer toe, an operation to straighten the toe may be necessary. This is often performed in conjunction with surgery for a bunion deformity. The surgical treatment of a hammer toe can consist of either cutting the tendons to relieve the pressure that causes the deformity, or fusing the toe so that it points straight permanently.
 Prevention
Prevention
Preventative treatment of hammertoe is directed toward the cause of the deformity. A functional orthotic is a special insert that can be prescribed by your podiatrist to address the abnormal functioning of the foot that causes the hammertoe. Functional orthotics can be thought of as contact lenses for your feet. They correct a number of foot problems that are caused by an abnormally functioning foot. Our feet, much like our eyes, change with time. Functional orthotics slow down or halt this gradual change in the foot. Often when orthotics are used for flexible hammertoes, the toes will overtime straighten out and correct themselves. Calf stretching exercises are also helpful. Calf stretching can help to overcome part of the muscle imbalance that causes the hammertoe.
Hammertoe Surgery Treatment
 Overview
Overview
A hammertoes is a deformity of the middle joint of a toe, producing a clenched, clawlike appearance in the affected digit. The tendons in the toe become abnormally contracted, causing the toe to bend downward, which, in turn, forces the joint to protrude upward. A mallet toe is a deformity in which the end joint of a toe becomes bent downward, so that the toe curls underneath itself. In either case the affected joints are stiff, and often the toe cannot be straightened out. Constant rubbing against shoes may furthermore cause a painful corn (a round patch of rough, thickened, calloused skin) to develop over the joint or at the tip of the affected toe. Hammer and mallet toes may occur in any toe, although the second toe is the most common site. These deformities are often painful and limit the toe?s range of motion-sometimes requiring surgery.
Causes
Poorly fitting shoes and muscle imbalances are the most common causes of hammertoe. When shoes are too narrow or do not accommodate the shape and size of your feet, they often contort the position of your toes. Choosing a shoe that fits is very important when it comes to avoiding foot problems like bunions or hammertoe. Having your toes bent for an extended period of time in a shoe that is too narrow or small forces your toes to adapt to the cramped space. With time, the muscles in your feet become accustomed to holding the flexed position of your toes, making it harder, or even impossible to straighten them.
 Symptoms
Symptoms
For some people, a hammer toe is nothing more than an unsightly deformity that detracts from the appearance of the foot. However, discomfort may develop if a corn or callus develops on the end or top of the toe. If pressure and friction continue on the end or top of the toe, a painful ulcer may develop. Discomfort or pain can lead to difficulty walking.
Diagnosis
Your healthcare provider will examine your foot, checking for redness, swelling, corns, and calluses. Your provider will also measure the flexibility of your toes and test how much feeling you have in your toes. You may have blood tests to check for arthritis, diabetes, and infection.
Non Surgical Treatment
Conservative treatment is limited to accommodation, not correction, of the deformity, though some patients find the relief they can get from these options to be more than enough to put off or even avoid surgery. These include better hammertoe Footwear. Shoe gear with a wider toe box and higher volume causes less friction to the toes. Toe Braces and Strapping. Some toe braces and strapping techniques take some pressure off the toes during gait. Custom molded orthotics can redistribute the forces through the tendons that control the toe, lessening the pain and extent of the deformity.The calluses on the toe and the ball of the foot can be shaved occasionally to reduce some pain and pressure, although they will return due to the constant deformity.
Surgical Treatment
There are generally two methods surgeons use to correct hammer toes, they are joint resection (arthroplasty) or bone mending (fusion), and the location where this is performed on the toe depends on where the toe is buckled. Its important to recognize that most of the surgical work involved the joints of the toe, not the joint of the ball of the foot. Sometimes a toe relocation procedure is needed when the joint of the ball of the foot is malaligned (subluxed or dislocated).
 Prevention
Prevention
Hammertoe can usually be prevented by wearing shoes that fit properly and give the toes plenty of room. Don?t wear shoes with pointed or narrow toes. Don?t wear shoes that are too tight or short. Don?t wear high-heeled shoes, which can force the toes forward. Choose shoes with wide or boxy toes. Choose shoes that are a half-inch longer than your longest toe. If shoes hurt, don?t wear them.
Hallux Valgus Symptoms
Overview
 Even though bunions are a common foot condition, they are probably the one with the most misconceptions. Many people suffer unnecessarily with the pain of bunions for years before seeking treatment out of fear about the ?surgery?. The good news is that most bunion pain can be resolved without surgery.
Even though bunions are a common foot condition, they are probably the one with the most misconceptions. Many people suffer unnecessarily with the pain of bunions for years before seeking treatment out of fear about the ?surgery?. The good news is that most bunion pain can be resolved without surgery.
Causes
Bunions are caused by pressure on the inside of the forefoot which causes the 1st metatarsal bone in the foot to migrating outwards. Biomechanical factors can contribute to the development of bunions for example if you over pronate where the foot rolls in or flattens excessively which causes the inside of the foot to rub against the shoe. Wearing high heeled shoes regularly also increases the risk of developing the condition . The pressure on the forefoot is increased considerably as the heel is raised up. Age is also a factor as the ligaments lose strength as you get older.
Symptoms
The most common symptoms of foot bunions are toe Position, the toe points inwards towards the other toes in the foot into the hallux adbucto valgus position and may even cross over the next toe. Bony Lump, swelling on the outer side of the base of the toe which protrudes outwards. Redness, over the bony lump where it becomes inflamed. Hard Skin, over the bony lump known as a callus. Pain, it is often painful around the big toe, made worse by pressure on the toe and weight bearing activities. Change in Foot Shape, Your whole foot may gradually change shape for example getting wider. Stiffness, the big toe often becomes stiff and may develop arthritis. Foot bunions are more common with increasing age. They develop gradually overtime from repeated force through the big toe and left untreated, become more pronounced with worsening symptoms.
Diagnosis
Your doctor will ask questions about your past health and carefully examine your toe and joint. Some of the questions might be: When did the bunions start? What activities or shoes make your bunions worse? Do any other joints hurt? The doctor will examine your toe and joint and check their range of motion. This is done while you are sitting and while you are standing so that the doctor can see the toe and joint at rest and while bearing weight. X-rays are often used to check for bone problems or to rule out other causes of pain and swelling. Other tests, such as blood tests or arthrocentesis (removal of fluid from a joint for testing), are sometimes done to check for other problems that can cause joint pain and swelling. These problems might include gout , rheumatoid arthritis , or joint infection.
Non Surgical Treatment
Non-surgical treatments for bunions may include wearing shoes that fit and that have adequate toe room. Stretching shoes professionally to make them larger. Putting bunion pads over the bunion to cushion the pain. Avoiding activities that cause pain, such as being on your feet for long periods of time. Taking over-the-counter pain relievers when necessary, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDS) like ibuprofen. Using ice to provide relief from inflammation and pain. Using custom-made orthotic devices. 
Surgical Treatment
Surgical treatment for bunion deformities usually involves an osteotomy, a procedure in which a cut or cuts are made in the affected bone or bones to restore proper alignment. Different techniques are used depending on the type of deformity; selection is guided by the degree of deformity present and the goals of preventing recurrence and achieving the most rapid recovery possible. Some of the more common procedures are. The distal chevron osteotomy: a procedure in which a v-shaped cut is made at the toe end of the first metatarsal. This surgery is appropriate for individuals who have a congruent deformity, one in which there is a painful prominence at the base of the toe, but the joint is still well aligned. Absorbable pins are placed in the metatarsal to maintain alignment during healing. The Scarf or Ludloff osteotomy: in this procedure, a more extensive cut is made higher up in the metatarsal to correct a moderate incongruent deformity and metatarsus primus varus. Screws are used to maintain alignment during healing. The crescent osteotomy: a procedure in which a curved cut is made at the base of the metatarsal is appropriate for patients with more severe metatarsus primus varus and, therefore, require more correction. Screws or pins are used to maintain alignment. The Lapidus procedure: individuals who have severe deformity, instability of the first ray, with a loose metatarsal-tarsal joint (located in the mid-foot) may not get enough correction from an osteotomy alone. Moreover, the looseness of the joint may lead to recurrence or be causing pain on the ball of the foot because the first metatarsal is floating up, allowing for excessive weight to go to adjacent metatarsals (commonly the second and the third). In such cases, the metatarsal-tarsus joint is fused to provide lasting stability. Screws are used to maintain alignment. The loss of motion from the fusion is small and does not significantly limit motion of the big toe. Patients undergoing bunion surgery are given an ankle block that anesthetizes the foot from the ankle down. Depending on individual preference, a sedative may be given as well and the patient can be as sedated as they wish. All bunion surgeries may be done on a same-day basis, eliminating the need for hospitalization.
What Does Overpronation Of The Feet Mean
One of the most common causes of foot and leg discomfort is a condition known as over pronation. Normal pronation, or "turning inward", of the foot is necessary as the foot adapts to the ground. With over pronation, however, the arch flattens, collapses, and soft tissues stretch. This causes the joint surfaces to function at unnatural angles to each other. When this happens, joints that should be stable now become very loose and flexible. At first, over pronation may cause fatigue. As the problem gets worse, strain on the muscles, tendons, and ligaments of the foot and lower leg can cause permanent problems and deformities.

Causes
There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
Because pronation is a twisting of the foot, all of the muscles and tendons which run from the leg and ankle into the foot will be twisted. In over-pronation, resulting laxity of the soft tissue structures of the foot and loosened joints cause the bones of the feet shift. When this occurs, the muscles which attach to these bones must also shift, or twist, in order to attach to these bones. The strongest and most important muscles that attach to our foot bones come from our lower leg. So, as these muscles course down the leg and across the ankle, they must twist to maintain their proper attachments in the foot. Injuries due to poor biomechanics and twisting of these muscles due to over-pronation include: shin splints, Achilles Tendonitis, generalized tendonitis, fatigue, muscle aches and pains, cramps, ankle sprains, and loss of muscular efficiency (reducing walking and running speed and endurance). Foot problems due to over-pronation include: bunions, heel spurs, plantar fasciitis, fallen and painful arches, hammer toes, and calluses.
Diagnosis
You can test for pronation by looking at the leg and foot from the back. Normally you can see the Achilles Tendon run straight down the leg into the heel. If the foot is pronated, the tendon will run straight down the leg, but when it lies on the heel it will twist outward. This makes the inner ankle bone much more prominent than the outer ankle bone.
Non Surgical Treatment
Supportive orthotics in the shoe is a method commonly implemented to treat many common running injuries associated with pronation. An advantage of orthotics is that they often allow the sufferer to continue to participate in athletic activity and avoid other treatment options that could be potentially costly and time consuming. Seventy-five percent of injured runners are successfully treated with the prescription of orthoses. Orthotics are the most effective treatment for symptoms that develop from unusual biomechanics within the body such as overpronation, resulting in either great improvement or complete healing of the injury in about half the cases.
Surgical Treatment
Depending on the severity of your condition, your surgeon may recommend one or more treatment options. Ultimately, however, it's YOUR decision as to which makes the most sense to you. There are many resources available online and elsewhere for you to research the various options and make an informed decision.
Calcaneal Apophysitis In Grown Ups
Sever?s disease occurs in children when the growing part of the heel is injured. This growing part is called the growth plate. The foot is one of the first body parts to grow to full size. This usually occurs in early puberty. During this time, bones often grow faster than muscles and tendons. As a result, muscles and tendons become ?tight.? The heel area is less flexible. During weight-bearing activity (activity performed while standing), the tight heel tendons may put too much pressure at the back of the heel (where the Achilles tendon attaches). This may injure the heel.
Causes
Severs disease is caused by repetitive excessive force to the growing area of the heel bone, causing injury to this area. The calf muscles (soleus and gastrocnemius) are attached by the Achilles tendon to the calcaneus (heel bone). They exert a huge force during running , jumping and landing. In children, there is a growing area in the heel bone called the apophysis and is made of relatively weak cartilage. If there is excessive force at this relatively weak point damage occurs. This excess force can be caused by a number of factors. During the adolescent growth spurt the bones grow very quickly. The muscles do not grow out at the same rate as the bone grows and so can become very tight. The calf muscles generate huge forces when they are used to run, jump and land. This force is transmitted to the calcaneal apophysis (growth area). The gastrocnemius muscle spans both the ankle and knee joint. Tightness of this or any other muscles of the lower limb (hamstring or quadriceps) cause extra force at the growing (weak) area. In active children, who undertake a lot of exercise, the repetitive high force causes damage. If your child has poor biomechanics due to poor lower limb alignment (often caused by flat feet), the muscles of the lower limb have to work excessively hard and this can cause increased force at the tibial tubercle.
Symptoms
The typical patient is a child between 10 and 13 years of age, complaining of pain in one or both heels with running and walking. The pain is localized to the point of the heel where the tendo-Achilles inserts into the calcaneus, and is tender to deep pressure at that site. Walking on his toes relieves the pain.
Diagnosis
A physical exam of the heel will show tenderness over the back of the heel but not in the Achilles tendon or plantar fascia. There may be tightness in the calf muscle, which contributes to tension on the heel. The tendons in the heel get stretched more in patients with flat feet. There is greater impact force on the heels of athletes with a high-arched, rigid foot. The doctor may order an x-ray because x-rays can confirm how mature the growth center is and if there are other sources of heel pain, such as a stress fracture or bone cyst. However, x-rays are not necessary to diagnose Sever?s disease, and it is not possible to make the diagnosis based on the x-ray alone.
Non Surgical Treatment
The aim of treatment is to reduce the pain and inflammation when gently stretch the muscles. There is likely to be no magic instant cure and the young athlete may have to be patient while they grow. Rest and apply ice or cold therapy to the heel. Do not apply ice directly to the skin but wrap in a wet tea towel to avoid ice burns. Rest from activities which cause pain. If running and playing football makes it worse then reduce or stop this activity and try cycling or swimming to maintain fitness. A temporary measure is to insert a heel pad or heel raise into the shoes. This has the effect of raising the heel and shortening the calf muscles and so taking the strain off the back of the heel. However long term use of a heal raise may shorten the calf muscles when they need stretching. Stretch the calf muscles regularly. Stretching should be done pain free and very gently with this injury. See a sports injury professional who can advise on treatment and rehabilitation.
Recovery
Sever?s disease is self-recovering, meaning that it will go away on its own when the foot is used less or when the bone is through growing. The condition is not expected to create any long-term disability, and expected to subside in 2-8 weeks. Some orthopedic surgeons will put the affected foot in a cast to immobilize it. While symptoms can resolve quickly, they can recur. Sever's disease is more common in boys than girls the average age of symptom onset is nine to eleven years.